While Crohn’s disease is a condition with both physical and mental consequences, it’s totally possible to live well when living with Crohn’s.
We spoke to one of Sidekick’s special health coaches, Jonna. As part of Sidekick’s IBD programs, Jonna works directly with people living with Crohn’s disease, providing them with personalized support and advice during their journeys.
Sidekick has created two programs for people living with inflammatory bowel diseases; Crohn’s and Ulcerative Colitis. This article specifically focuses on Crohn’s disease. To find out more about Sidekick’s IBD programs, visit this page.
Keep on reading to discover Jonna’s insight into how to manage the symptoms of Crohn’s disease and take back control of your health.
Hi, Jonna! Thank you so much for joining us on Living Well. Can you tell us a little bit about yourself?
Thank you for having me! I studied Health and Medical Psychology, through which I dived deep into the world of chronic conditions, including Crohn’s disease, especially from a psychological perspective.
During my studies, I realized that there is a huge need for people living with IBD to be supported holistically. This is because the impact that the condition has on a person’s life goes far beyond the physical symptoms.
I am so grateful to have been able to do exactly this as a coach in Sidekick’s IBD programs.
In your experience working as a coach in Sidekick’s Crohn’s program, what are some of the most common symptoms people living with the condition struggle with?
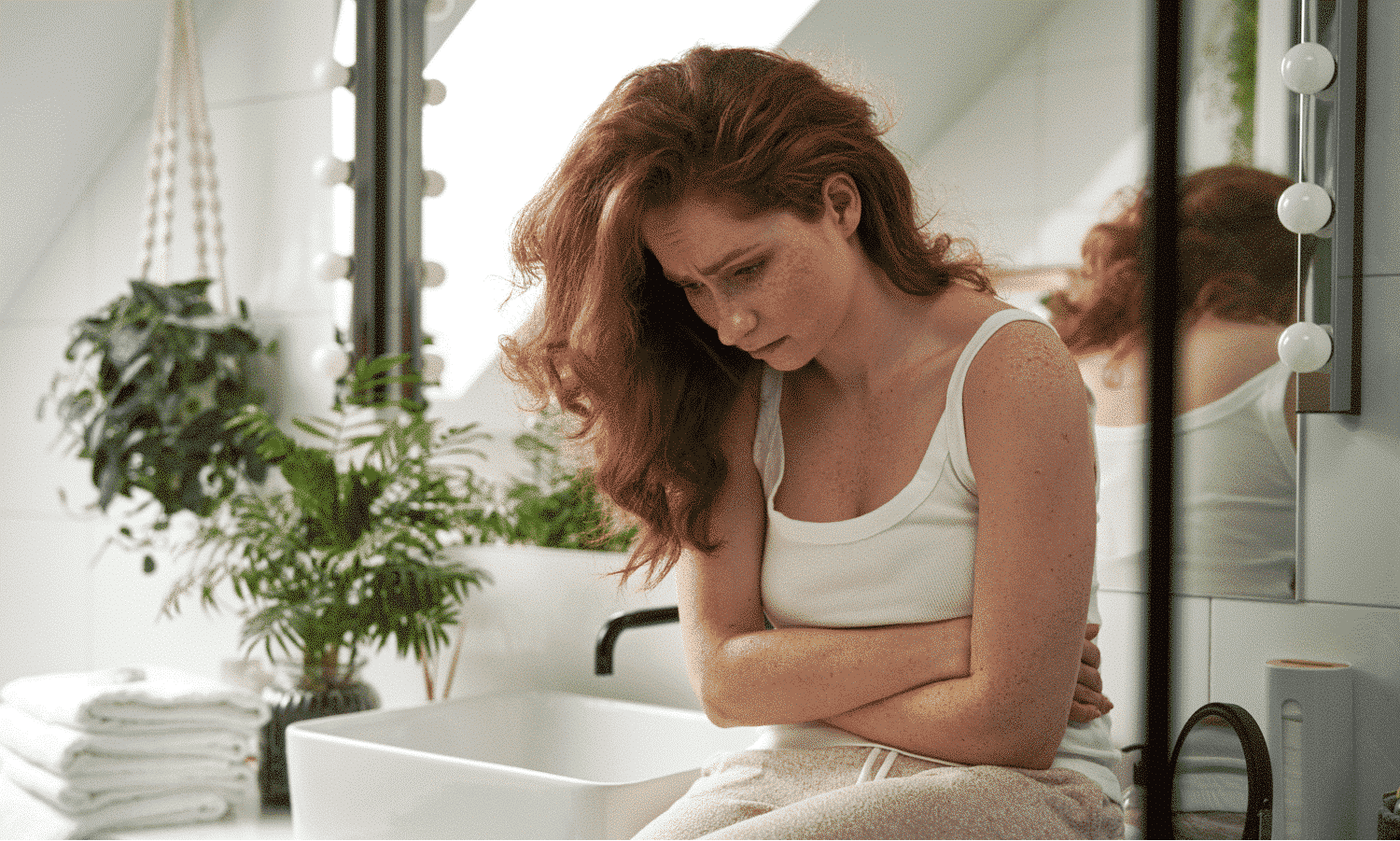
People living with Crohn’s often struggle with difficult physical symptoms, such as diarrhea, abdominal cramps and pain, bloody stools, urgent and frequent bowel movements, reduced appetite, weight loss, and mouth sores.
Some other symptoms that I hear about very commonly and what I’ve noticed based on the users’ activity in the Sidekick app are lack of energy, fatigue, high stress, and sleeping problems.
You can probably imagine how intertwined these symptoms can be.
For example, having abdominal pain and other troublesome physical symptoms most likely increases your stress levels. You may have to take sick leave from work, or you have to cancel meetings with friends and fear they don’t understand why.
This, in turn, might make you feel even more worn out and tired, both emotionally and physically. What’s more, because of this high stress and pain, you might still experience trouble falling asleep.
In fact, when asking IBD patients about the role their condition plays in their life, they often say that the condition “affects everything” in their lives.
Can you tell us about some of the mental health side effects of the condition?
Firstly, being diagnosed with a chronic condition means that you have to cope with the frustrating fact that the condition isn’t going anywhere.
Crohn’s disease especially can be quite unpredictable in nature, which can make people feel that they have no control over their own bodies or health.
It may be hard to find the motivation to keep following your treatment plan day after day and to remain hopeful about the future. People may also feel exhausted trying to find the right diet and medication that works for them.
It is also common for IBD patients to feel embarrassed about their condition or symptoms. It may be difficult to communicate with other people without going into ‘too much’ detail.
There are a lot of taboos around people’s toilet behaviors that may not be considered appropriate to talk about in certain social situations.
People living with IBD may also feel that other people don’t understand what it is like to live with the condition. In fact, they might start avoiding social situations due to pain, fatigue, and concerns about not making it to the bathroom in time or needing to use the bathroom multiple times.
People living with IBD may also feel that other people don’t understand what it is like to live with the condition. In fact, they might start avoiding social situations due to pain, fatigue, and concerns about not making it to the bathroom in time or needing to use the bathroom multiple times.
The condition might affect your body image, too. You may be, for example, losing weight due to your disease or experience swelling due to steroids. It may be very hard to see your body change in unwanted ways. Sometimes, other people may make the situation worse with inconsiderate comments.
Another much-talked-about mental health side effect is stress. Although stress doesn’t specifically cause Crohn’s disease, it can trigger flare-ups and relapse in Crohn’s disease.
Understandably, worsening IBD symptoms often lead to even more stress, easily making it a vicious cycle. This is why stress management is so important in minimizing the effect Crohn’s has on the individual’s life.
It has also been found that people with IBD are at an increased risk of developing anxiety and depression. Some research has found that anxiety and depression might be even two to three times more likely to occur in IBD patients compared with the general population.
If you notice these feelings of anxiety, depression, or overwhelming stress, know that these feelings are common and you are not alone. Do not ignore them, and seek help from a mental health professional.
Your mental health is just as important to take care of as your physical health.
Finding a nutrition plan that works for you is a big part of managing Crohn’s disease. Can you explain why this is so important?
A nutrition plan that works for you helps you prevent weight loss and malnutrition and helps maintain and improve general fitness.
During a flare-up, it’s important to avoid foods that may cause worsening of the symptoms.
A normal diet during a flare-up can make diarrhea and stomach aches worse, and some foods, in particular, can be linked to the symptoms.
I want to emphasize that these reactions to food are individual, and the diet of the active phase of the condition should be planned together with a dietitian or other health care professional.
What tips can you offer people living with Crohn’s disease to ensure their diet is versalite and nutritious, particularly during a flare-up?
I think the emphasis here is indeed on eating as varied as possible. That is, sometimes people with Crohn’s have to follow a very strict diet during a flare-up, but even then, it is good for recovery to eat regularly, eat in a variety of ways – within the limits of your diet – and take care of adequate hydration.
During a flare-up, you should eliminate high-fiber and hard-to-digest foods. Easily digestible and liquid food such as soups can be preferred.
Suitable drinks are rather dilute drinks containing salts and sugars, whereas caffeinated, carbonated, and alcoholic drinks should be avoided.
In remission, it is good to try your excluded foods again so that your diet remains as varied and nutritious as possible.
A diet low in fermentable carbs, called the FODMAP diet, is often recommended to manage irritable bowel syndrome (IBS). It can be helpful for stomach problems in the remission phase of IBD patients.
Again, consultation with your doctor and dietitian about dietary changes is important. They can help you find out what works best for you.
What are some ways that people living with Crohn’s disease can deal with the unpredictable nature of the condition?
Living with Crohn’s disease can diminish the feeling of control that you have over your own body.
To deal with the unpredictable nature of the condition, I think it’s important to identify and practice control in the areas of your life that you can control and, on the other hand, accept the areas of life that are out of your control.
You may, for example, not be able to control the timing and severity of a flare-up, but you can take control of how to deal with it.
For example, you can actively practice stress management techniques; you can learn to plan and prepare nourishing meals; you can make sure to follow your treatment plan; and, importantly, you can ask for help when you need it.
Another thing that I would recommend to anyone is finding other people that live with the same condition. This will allow you to share your experiences and worries, as well as receive the kind of understanding and support that only people that have experienced similar things can give you.
Merely realizing that you are not the only one struggling with these problems can be very comforting.
And finally, what behavioral changes can people living with Crohn’s practice to improve their overall quality of life?
Good eating habits and an overall healthy lifestyle promote the quality of life of people with Crohn’s disease. Eating habits are not so much about what you eat but how you eat.
When living with Crohn’s disease, it is important to eat calmly and to chew carefully, for example. By chewing well, you can prevent digestive problems and help in nutrient absorption.
In addition, eat small portions regularly, for example, five times a day. Give your gut enough time to rest in-between meals by avoiding snacking.
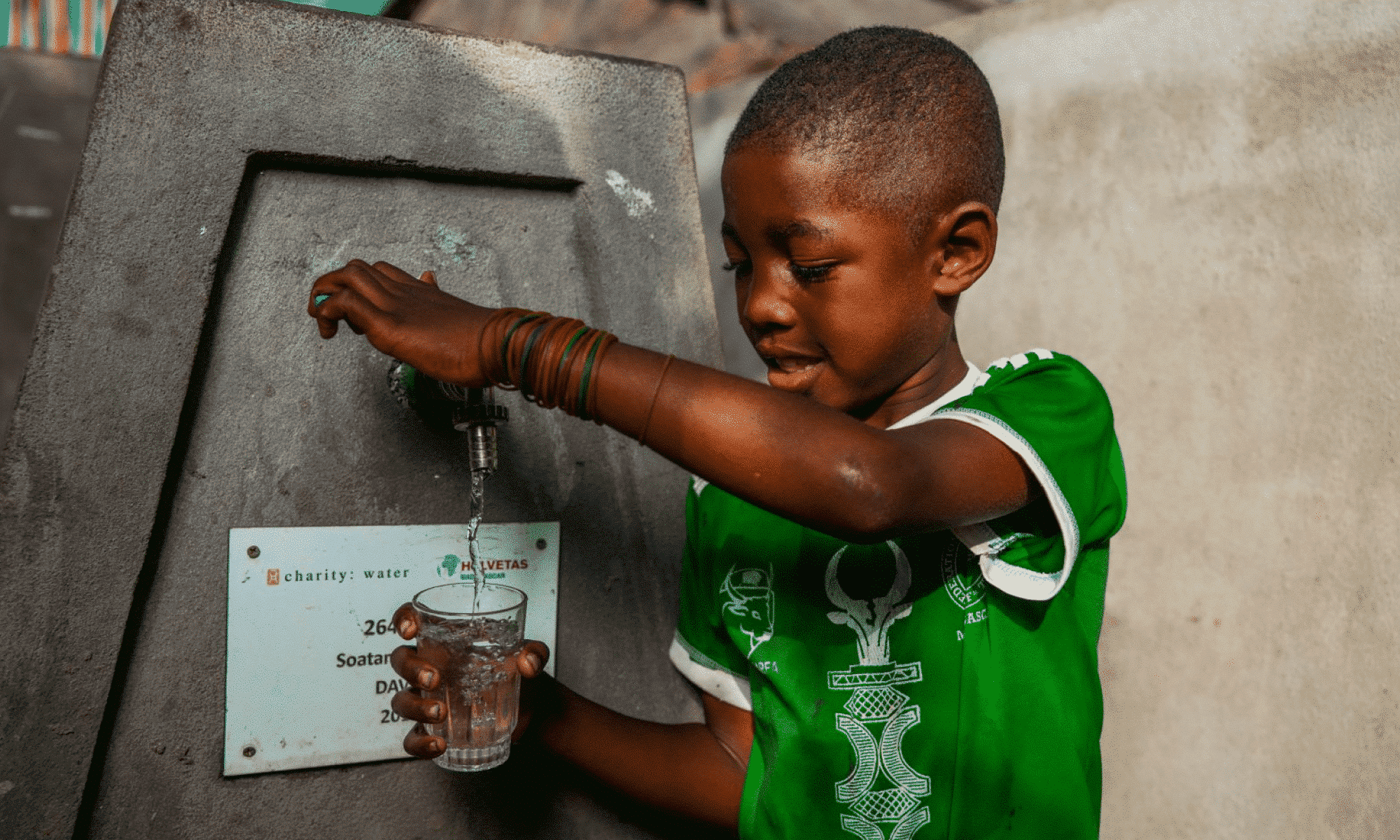
Take care of adequate hydration by drinking 1-1.5 liters of water during the day. Practicing “mindful eating” can help you be aware of the food and drink you put into your body. It involves observing how the food makes you feel, what emotions and thoughts arise, and the signals your body sends about taste, satisfaction, and fullness.
Regarding lifestyle factors, quitting smoking is one of the most important things that people with Crohn’s disease can do for their health and quality of life. Smoking can make the condition worse.
People with Crohn’s disease who smoke may find that they have more severe symptoms and complications, increasing the need for steroids, immunosuppressants, and re-operations.
Other lifestyle factors that contribute to improved quality of life are regular exercise, stress management, and taking care of adequate sleep and rest. Exercise not only helps your digestive tract work more efficiently, but it can also help reduce stress due to the release of endorphins, the “feel-good hormones.”
There are so many ways to move your body, so choose an exercise you actually enjoy! You may want to ask a friend or family member to join, so this way, you also take care of your social needs.
There are, of course, many other ways to manage stress. For some people, spending time with loved ones and talking about their worries works best.
You may want to try mindfulness exercises, meditation, yoga, or journaling. Or, it could just be reading a book, listening to music, or whatever you enjoy doing and find relaxing. Do what works for you.
When it comes to rest and sleeping, consistency is key. Indeed, you’ll sleep better if you stick to a routine. Set a time for getting up and going to bed on weekdays and on weekends.
Be also sure to give yourself enough time to wind down before bed. Make sure to check the temperature and lighting of your bedroom, only consume caffeinated drinks early during the day, and avoid napping.
If you’re living with Crohn’s disease or are caring for someone who is, be sure to explore our other articles on Crohn’s. We’ve got real stories from real people living with the condition as well as tips on how to reduce Crohn’s related stress. Discover more right here.