|
Getting your Trinity Audio player ready...
|
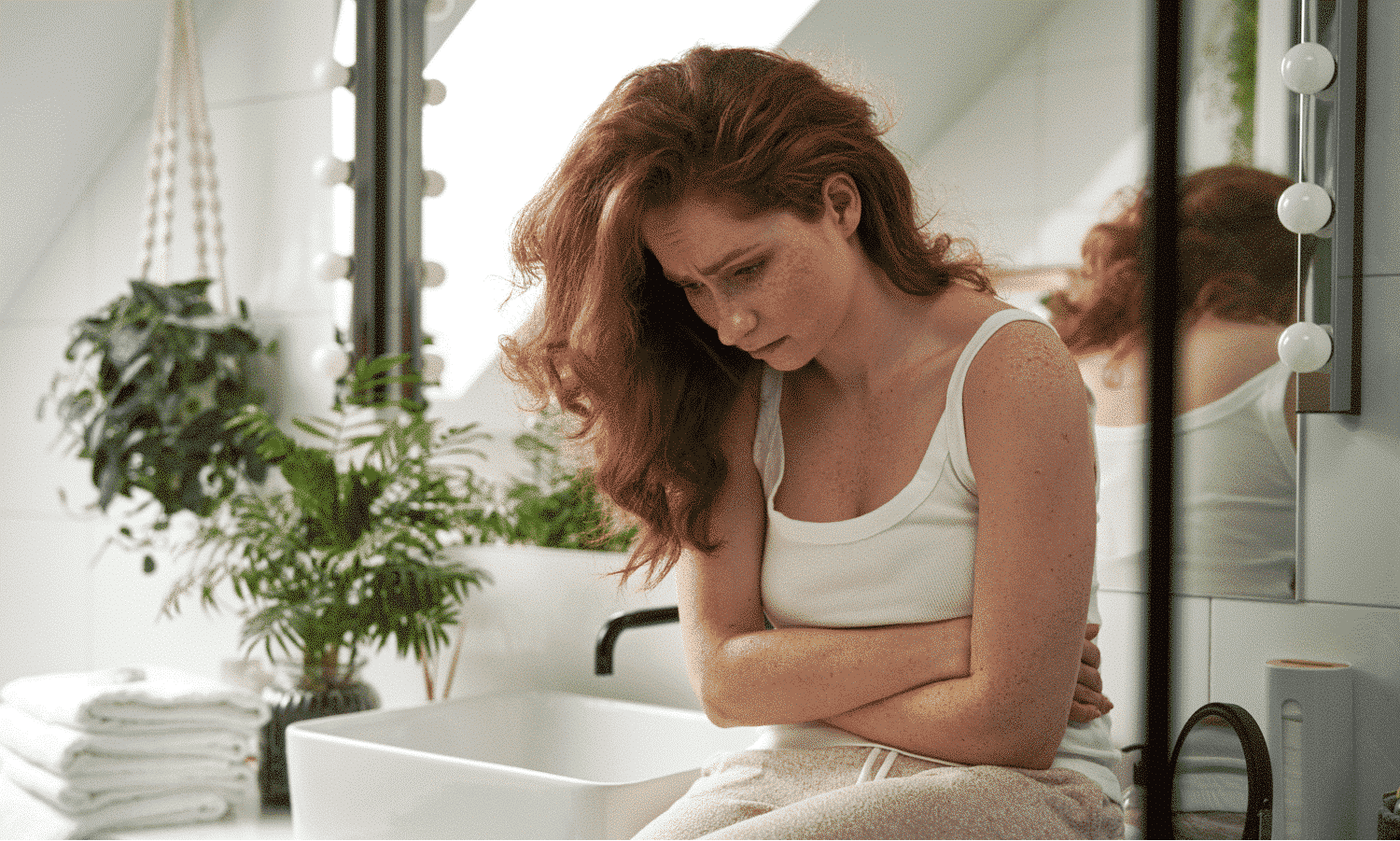
Stress can have a profound impact on our wellbeing. It can affect our bodies, thoughts, feelings, and behavior.
If you’re living with a chronic condition like Crohn’s disease, psychological stress may also make the symptoms of your condition worse. This can cause a vicious cycle because the symptoms themselves can be another source of stress.
But how can stress make Crohn’s disease worse? It could be down to something called the “brain-gut connection.” Your brain and gut are linked by the vagus nerve, a part of your nervous system that plays an important part in many functions, including your digestion, immune system responses, and mood.
Let’s start with the basics. Crohn’s is an inflammatory disease. Crohn’s related inflammation happens in the organs that food and liquid travel through as they’re digested (also called the gastrointestinal or GI tract). How you feel mentally can affect the way your digestive system functions too. For example, if you’ve ever been nervous about something and felt “butterflies in your stomach,” this could be down to the “brain-gut connection.”
For those living with an inflammatory disease such as Crohn’s, it’s important to know that, while the condition can’t be cured, it can be managed. Along with the treatment you receive from your doctor to reduce inflammation, you can also manage your stress in an effort to control your symptoms and improve your overall quality of life.
Keep on reading to discover tips on how to manage your Crohn’s related stress.
What can trigger Crohn’s disease-related stress?
Many things might trigger stress when you’re living with Crohn’s disease, but the important thing to remember is that you’re not alone, and others might be experiencing the same worries as you. Here are some possible stressors that could be getting you down:
Flare-ups
From diarrhea and abdominal pain to frequent and urgent bowel movements and fever, the symptoms of a Crohn’s disease flare-up can cause stress, and the unpredictability of symptoms may also make stress worse.
Unfortunately, not only can flare-ups cause stress, but stress can cause flare-ups. Therefore, it’s important to practice stress management to minimize this. Keep reading to find out how.
Eating out
For those living with an inflammatory bowel disease like Crohn’s, eating out can trigger feelings of anxiety.
If your symptoms are in a flare state, you might be worried that eating out will make the symptoms worse, or if you’re in remission (the periods of time when you have no current symptoms), you may feel anxious about eating something that will trigger a flare-up.
Bathroom anxiety
Due to the unpredictable nature of Crohn’s disease, you’ll never know when diarrhea will strike.
This could make you nervous about going out because you may suddenly need quick access to a bathroom, and your only choice might be a public restroom or a friend’s bathroom.
This is not ideal when dealing with an unexpected bout of diarrhea and could make you feel anxious or stressed.
Social stigma
Dealing with other people’s perceptions and ideas about your condition might make you feel isolated and stressed. You may be worried that people see you or treat you differently, and therefore not feel understood or supported.
How to manage stress when living with Crohn’s disease
Stress management when living with Crohn’s disease could help you deal with the mental and physical challenges it brings, such as flare-ups.
Here are some tips that might help to reduce feelings of stress and anxiety:
Practice preventing flare-ups
Crohn’s disease is, by nature, unpredictable, and you may experience symptoms and flare-ups at a moment’s notice which, of course, can feel stressful.
But, there are some things you can do that could prevent flare-ups and reduce stress, such as:
Eating and drinking right
Some foods could be difficult for you to digest and therefore, cause flare-ups. Here are some foods and drinks you could try avoiding or consuming in moderation:
- Wholegrain foods such as whole wheat pasta and whole wheat bread
- Red meat, sausages, and dark meat poultry
- Dairy products such as butter, cream, full-fat dairy, and margarine
- Coffee, black tea, soda, and alcohol
- Garlic, jalapeños, wasabi, white/yellow/purple onions, chili powder, cayenne pepper, black pepper, and paprika
- Broccoli, cabbage, cauliflower, and artichokes
- Apples with skins, cherries, peaches, and plums
Instead, try eating and drinking more of the following:
- Potatoes, white pasta, rice and rice pasta, polenta, oatmeal, and gluten-free bread
- Fish, tofu, eggs, shellfish, peanut butter, and white meat poultry
- Milk, yogurt, and cheese made from soy, coconut, almond, flax, or hemp
- Water and non-caffeinated herbal tea
- Turmeric, ginger, cumin, mustard, and fresh herbs
- Carrots, spinach, peeled cucumbers, bell peppers, pumpkin, and squash
- Bananas and cantaloupes
* Please note that the above are suggestions. There is not enough research to support their effectiveness.
Everyone reacts to various foods in different ways, so try writing in a food journal to keep track of anything that disagrees with your body. Sometimes, it’s hard to pinpoint an exact food or ingredient that triggers your condition; recording your meals might help you narrow this down and find the common problem.
Exercise
Regular physical activity may reduce inflammation, which may result in fewer flare-ups. Choosing exercises that you enjoy might make you more likely to stick to them. Low-impact choices like walking, biking, swimming, and yoga are good places to start.
Of course, if you’re not feeling great or are in the middle of a flare-up, resting is also important. Don’t push yourself, as this could leave you feeling more stressed.
Keep up with your medication
If your doctor has prescribed medication, it’s important that you stick to it along with any instructions and advice they’ve given you. This still applies even if you’re feeling okay because the goal is that you keep feeling okay.
When you download a Sidekick program, you can use the medication reminder feature to help you keep track of when you need to take your medication.
Make dining out less stressful
If social events call for eating out, do some research ahead of time to manage your stress when the occasion arrives. Check out the menu online and see what dishes you can order that will potentially cause you the least problems. If you’re not sure about a certain dish, call the venue and ask.
When it comes to ordering, don’t be afraid to ask if you can make alterations to a certain dish. For example, request for a sauce to be added to the side instead of over the food just in case it’s a spicy one; ask for an ingredient to be grilled instead of fried; ask for specific ingredients to be removed from the dish if you know that they’re triggers.
Reduce bathroom anxiety
Worried about not knowing where the nearest restroom is if you go out? There are a few bathroom apps that can help you with just that. Before you head out, browse the app for the location you’ll be in and make sure you have a rough idea of how to get yourself to the nearest toilet, should the need occur.
The fact that everyone poops might not provide much comfort when you get a sudden urge to go. So, if you want to mask the sound in a public restroom, put a layer of toilet paper in the bowl. Or, if you’re at a friend’s house, run the tap. You might find that some toilets don’t have paper, so carry tissue or wipes with you, just in case.
Nervous about smells? If you’re at someone’s house, flush often to get rid of the source of the smell, or spritz the bowl with scented spray before you go to mask the odor.
And if you can, try to relax. If you’re using a public restroom, you’ll probably never see those people again. If you’re at someone’s house, try to remember that everyone really does poop, and they all know it’s not always pretty.
Write down your thoughts
Expressive writing, or journaling, may help you relax because it can clear your mind and allow you to release negative or stressful thoughts.
When you’re feeling stressed, it can be easy to forget about the things that are going well. Writing down positive events, personal victories, and happy thoughts is also important. This can remind you of the things you’ve overcome and help give you motivation for when times get tough.
If you want to start a journaling habit, try to find 15 minutes at the same time each day. Choosing a place where you won’t be distracted is best, and if pen and paper aren’t for you, try using a computer.
There are also journaling apps you can use on your tablet or phone – the more accessible you make it for yourself, the more likely it could be that you keep up the habit.
Find support
Prioritizing your mental health is important when dealing with a chronic condition. While talking to friends and family can give you comfort, you could also find relief in talking to other people with Crohn’s disease.
Look online for support groups that deal with inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis. The Crohn’s & Colitis Foundation has a community that offers support and resources to help make your daily life easier.
Crohn’s disease can correlate with feelings of anxiety and depression. So, if you’ve been dealing with stress and negative feelings for several weeks, we encourage you to see your doctor or another medical professional for advice.
If you want to discover more ways to deal with stress, check out this article on mindfulness and stress management.
If you live in Ireland, you have access to our Crohn’s disease program! From keeping track of your medication to discovering new ways to relieve symptoms and learning mindfulness techniques, your Sidekick has so much to offer – find out more here.