|
Getting your Trinity Audio player ready...
|
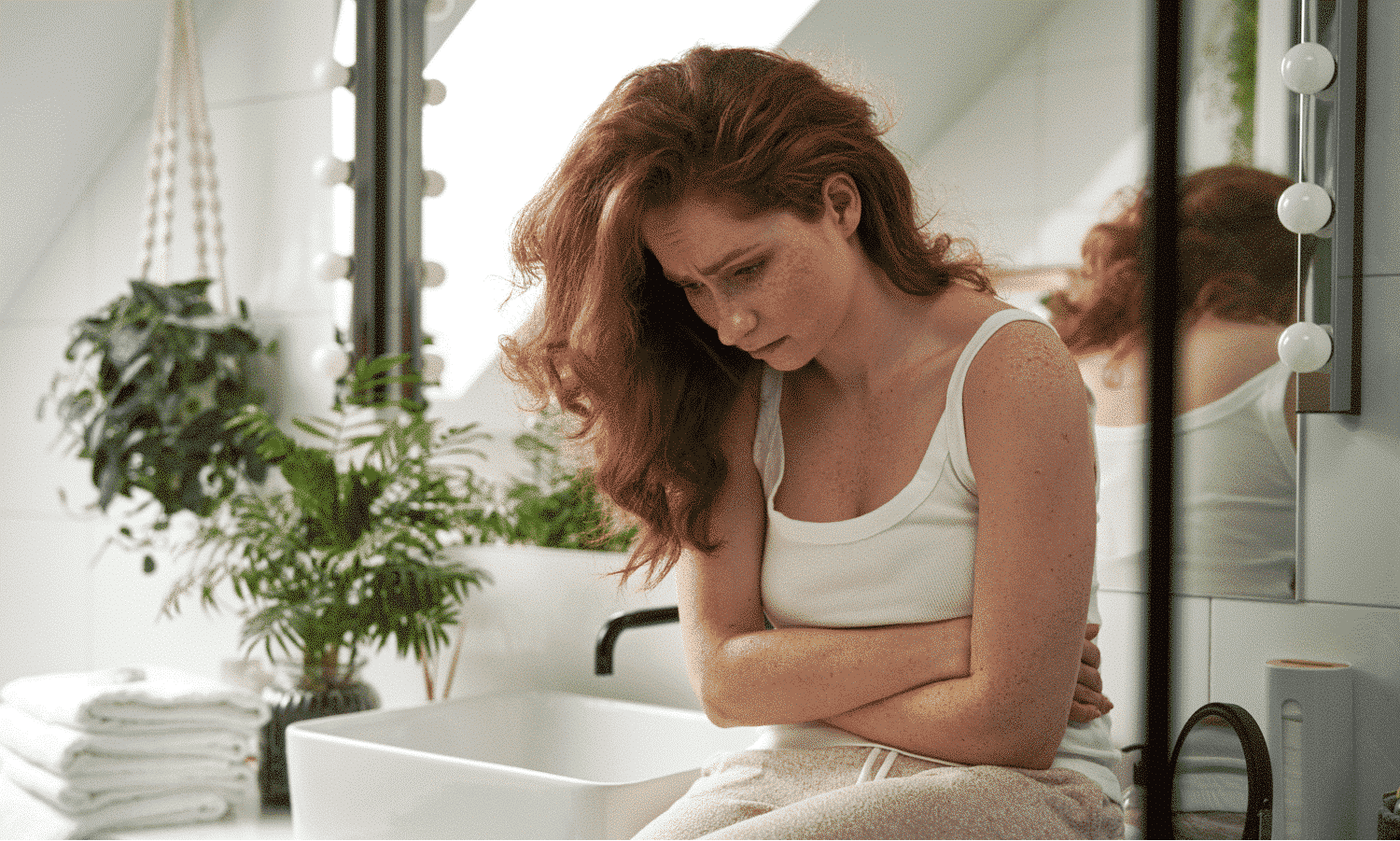
What do a toothache and stubbing your toe have in common? They’re both causes of pain! Yes, one might feel more painful than the other, but they’re both things that happen to our body that cause us discomfort.
The complicated thing about pain is that, to each and every person, it can feel different. To some, stubbing a toe can have them hopping around the room howling in agony, while to others, a quick grimace and a curse word follow, and then, back to business as usual.
This is why you need to be as clear and descriptive as possible with your doctor if you’re experiencing any form of pain. From how bad it is, to where it is, and everything in between, these details are what help doctors discover underlying problems and help when it comes to managing pain.
Here, we talk about some types of pain, how to describe your pain to your doctor and why it’s important to do so.
What are some different types of pain?
Before we get into how to talk about pain with your doctor, here’s a rundown of some of the types of pain bodies can experience.
Acute pain
Acute pain occurs suddenly and is brought on by a specific cause. It generally lasts for less than six months and eventually goes away once the root cause is treated or when the injury has healed. Common sources of acute pain include:
- Broken bones
- Surgery
- Dental work
- Labor and childbirth
- Cuts
- Burns
Chronic pain
Estimated to affect 50 million adults in the US, chronic pain is defined as lasting more than six months, even after the original injury has healed. Some examples of chronic pain include:
- Frequent headaches
- Nerve damage pain
- Lower back pain
- Arthritic pain
- Neck pain
- Muscle pain all over (such as fibromyalgia)
- Some joint pain (but keep in mind that not all joint pain is chronic)
Because of its draining effect on people’s quality of life, chronic pain can sometimes result in people developing symptoms of anxiety and depression, as well as other symptoms such as tense muscles, lack of energy, and limited mobility.
Nociceptive pain
Nociceptive (pronounced “noh-suh-sept-iv”) pain describes the pain felt in response to certain stimuli, like tissue damage or in anticipation of dangers like extreme cold. It can feel sharp, aching, or throbbing and can be caused by things like stubbing your toe, a sports injury, or dental work, to name a few.
Bruises, burns, fractures, and pain caused by joint damage, such as arthritis or sprains, are all injuries that can cause nociceptive pain.
Neuropathic pain
Neuropathic pain is caused by damage to or dysfunction of the nervous system and can appear to come out of nowhere instead of coming from a specific injury. Neuropathic pain can feel like:
- Burning
- Freezing
- Numbness
- Tingling
- Shooting
- Stabbing
- Electric shocks
There are many causes of neuropathic pain, such as:
- Diabetes
- Chronic alcohol consumption
- Accidents
- Infections
- Radiation
- Chemotherapy drugs
- Spinal nerve inflammation or compression
- Central nervous system disorders, such as multiple sclerosis or Parkinson’s disease
There are, of course, many other causes of these types of pain. If you’re experiencing a new pain or a continuing pain, we encourage you to visit your healthcare provider or contact your pain management specialist.
How can you describe your pain to your doctor?
Everyone experiences pain differently, so it can be hard to explain to your doctor how your pain feels, what kind of pain it is, or even where exactly it’s coming from. But, if you can describe your pain as clearly as possible, this will help your doctor to help you.
Here are some ways you can talk about pain, as well as some tips on how to record it.
Numeric rating scales (NRS)
Just like how we use a scale of 0-10 to rank movies, places, food, books, or how hard something is, it’s also very helpful for communicating how much pain we’re experiencing to our doctor.
Called a numeric rating scale (NRS), the numbers on the scale represent the amount of pain someone is feeling, with 0 being none, 1/2/3 being mild pain, 4/5/6 being moderately strong pain, 7/8/9/10 being severe pain – 10 being the worst pain you can imagine.
Pain scales are commonly used in healthcare and are very helpful for doctors to understand the severity of someone’s pain.
Descriptive words
Sometimes, if a person is in pain, it’s hard to describe this verbally. So, if you can familiarize yourself with some common “pain words,” your doctor can get a clearer idea of what and how serious the underlying issue is.
- Burning – a pain that feels hot.
- Sharp – pain that feels sudden and severe.
- Dull – pain that’s not severe but lasts for a long time.
- Intense – a feeling of unbearable pain.
- Aching – similar to dull. Pain that’s not severe but continues giving discomfort.
- Cramping – sudden feelings of sharp pain or contraction-like pain.
- Nagging – not severe but hard to get rid of, like a mild but annoying headache.
- Shooting – sudden severe pains that move through the body.
- Stabbing – sudden feelings of strong pain that may feel very local to one area.
- Gnawing – a dull but constant pain.
- Gripping – sudden pain that also may contract.
- Pressure – a pain that feels heavy or tight in a certain area.
- Heavy – a feeling of uncomfortable weight on a part of the body, maybe it’s hard to move too.
- Tender – a pain that feels sensitive to the touch or to movement.
- Sensitive – similar to tender. A part of your body might be painful to move or touch.
- Prickly – a pain that almost feels like tingling.
- Stinging – a sudden burning pain in your eyes or on your skin.
- Agonizing – very, very painful.
- Crippling – causing so much pain, maybe it’s hard to move or do daily activities.
- Itchy – any uncomfortable feeling on your skin that makes you want to scratch.
- Tight – feels like a part of your body is being squeezed hard.
- Raw – when your skin feels very sore and sensitive.
The more detail you can give your doctor, the quicker and better they could be able to diagnose your pain and offer advice. This leads us nicely on to…
Keep a pain journal
Staying proactive can be hard if you’re suffering, but keeping a pain journal is an excellent way of recording your symptoms, pain levels, and general feelings. If you don’t feel that you’re able to do this, ask a family member, friend, or other caregiver to be your scribe!
Some helpful questions to answer in your journal could be:
- When did the pain start?
- How long does the pain last?
- How does the pain feel? (Use the descriptive words above to help with this.)
- Is your pain tolerable?
- How severe is the pain? (This is where the trusty 0-10 pain scale comes in.)
- Where do you feel the pain? If you can’t tell where the pain is coming from specifically, write down the general area on your body.
- What triggers the pain?
- Is the pain worse in the morning/day/evening/when you’re trying to sleep?
- Does anything make the pain feel better/worse? What?
- Are you taking any medication to help? What and how often?
- Is the pain stopping you from doing your normal daily activities?
This valuable information can assist your doctor in making a more accurate diagnosis, so make sure to bring your pain journal along to your appointments.
Along with your journal, any other details you can think of when you’re talking to your doctor – no matter how small you think it is – could bring them closer to understanding the root cause and coming up with a treatment plan to ease your symptoms.
Why is it so important to describe your pain to your doctor?
While your doctor knows your medical history, only you know your body best. If something doesn’t feel right or “normal”, it’s important to find out if there’s a problem.
It’s natural to feel nervous or hesitant when talking about something that’s causing you distress, especially pain. You may be worried that something might be wrong and try to play down your symptoms – this won’t be helpful for you or your doctor.
For any healthcare provider to fully understand what you and your body are experiencing, no detail is too small or “irrelevant”. Something you mention casually might be useful in helping them discover what’s causing you trouble – it all counts.
This is where being your own health advocate is key; express your concerns fully with your doctor, including the details of any pain or symptoms, and feel free to ask questions if you’re unsure of anything your doctor says. Aim to be confident in how you talk about your healthcare and worries; it’s your body and therefore your right to seek the best support for it. You can read more on the importance of patient advocacy right here.
As well as seeking guidance from your healthcare provider, we also encourage you to explore our programs. Sidekick’s programs feature plenty of pain management tips, such as mindfulness and behavior modification techniques.
While experiencing pain can be a daily reality for people living with chronic conditions, you have the power to take back control of your health and live your life without being defined by your pain or your condition.